Tags
adrenal-fatigue, anger, anxiety, childbirth, chronic-fatigue, chronic-pain, health, mental-health, pelvic-congestion
NOTE: This is part six in a blog series on my 15-year journey to better health. Want to start from the beginning? Click here to start with part one.
Finally, I encounter a few providers who diagnose and resolve a problem that leads to improvement.
With the first light, hope whispers that even the longest night must yield to the coming day.
–Unknown
In the letter informing me that the founder of the PT clinic—who had actually been helping me—had retired, I was referred to another provider at the same clinic. Due to my earlier issues with another provider there, I was hesitant to try anyone else, but I was still desperate for help, so I decided to give it a shot.
A Question to Set Me on the Right Path
This new physical therapist was a young guy—very kind, unlike the first one I’d seen—but he didn’t seem to have the same “magic” the founder did. I went to him for 2-3 weeks, and was telling him more of my story each time. In the last appointment I had with him, I was saying how my leg pain would temporarily go away from PT or massages or other treatments, but would always come back. He paused for a moment after that information, and then asked me if I had any issues with my stomach. I responded that I’d dealt with numerous stomach issues over the years, but had never truly resolved them. He suggested that I go see a gastroenterology (GI) doctor, suggesting that an underlying problem in that lower stomach / pelvic region could result in recurring hip and leg pain.
I had just finished taking my son to a GI doctor as he was having a lot of stomach issues, and through that process we found a clinic and some doctors we liked. I was familiar with the testing they may do, and knew what it would cost, so I decided to go in for me. After my initial appointment, they recommended a number of the same tests–images, colonoscopy, some drinking and breath test, etc.
I held my breath when I went back in to hear the results. Knowing I’d been struggling with my stomach for years, and knowing my son had some real issues diagnosed this way, I was hopeful to find the same. Maybe then I could have a path to getting better, and maybe then I could stop feeling like I was crazy. Unfortunately, in the follow up the GI doctor told me my digestive system looks great–no issues there based on his tests (all normal!). My heart dropped to the floor.
But, he added, there was something abnormal in the images that he thinks I should follow up on. They showed that my ovarian veins were very enlarged. He explained that this could be indicative of a condition called Pelvic Congestion Syndrome (PCS). He added that this is not an issue he can help with, but suggested I maybe seek input from an OBGYN. I thanked him, hopeful to have a new lead, and we wrapped up.
A Potential New Diagnosis
When I got home, I hit the web to research. The more I read about PCS, the more I started to believe this was very likely causing me problems. I found several studies and a few personal accounts that mentioned it resulted in hip pain or leg pain. I found that it is very common to occur in women who birth one or more children, especially if they are hyper-mobile / hyper-flexible, as that implies a connective tissue disorder that can occur in the veins as well (I’m hyper mobile). Another interesting finding from my research was that the type of doctor to help with this condition is not an OBGYN, but a vascular radiologist. While reading, I suddenly remembered that I had images of my pelvis taken years before. Multiple times. That I’d even had a pelvic laparoscopy back in 2011 (discussed in part 3).
I rushed to my office and dug through my medical records. When I found the laparoscopy report, I noticed a note on the images. My ovarian veins were circled, and there was a comment next to it: “varicose veins?” And this was something that was not mentioned to me when that procedure was done, even though I was in there for pelvic pain. It was now 2019… this was a problem I’d had and had been detected eight years earlier. I fell to the floor and wailed in disbelief. If this is the cause of my hip and leg pain, I’d wasted eight years suffering. I had tried to get help, and they had found a problem, but they ignored it.
I looked back at the CT scan my internal medicine doctor took in 2014 and noticed it was mentioned there as well (discussed in part 4). This was when I re-discovered that she had actually told me about the finding, and had recommended back then for me to go to an OBGYN for follow up… but I didn’t–maybe I forgot, or maybe I dismissed it… regardless, I was sick over how much time I’d lost.
Finding the Right Provider & Treatment
I scheduled appointments with three leading vascular radiologists in my area—I wasn’t willing to risk another misdiagnosis or unnecessary treatment. After meeting with the first two, I’d learned that it was confirmed that I had PCS, which is really another term for enlarged varicose veins in your pelvic region–for me, my ovarian veins. Congestion meant the blood was not flowing as it should (like varicose veins in the leg).
Another thing I learned from these providers was that the procedure to correct the issue was not covered by insurance, and would cost about $90,000. Apparently, correction of Pelvic Congestion Syndrome was supposed to improve pelvic pain, but didn’t have a significant positive outcomes according to insurance, so it was no longer covered. Even though those same insurance agencies covered the fixing of varicose veins in the leg, and the data was clear that varicose veins in the leg cause pain. I was so angry, I thought for sure this would be another dead end (there’s no way for me to come up with $90k), but I had one more doctor to see.
My appointment with the third vascular radiologist was downtown, at the University of Minnesota. The doctor there ran a new test I’d never had before–a venogram, where they basically take a video of my blood flow for 10-20 minutes, and during that, have me intermittently bear down to simulate the pressure my body would feel when I was standing upright or exerting myself.
When I went back in a few weeks later to discuss the results, the doctor was almost giddy to explain. He said my results were almost the worst he’d ever seen.
When I went back in a few weeks later to discuss the results, the doctor was almost giddy to explain. He said my results were almost the worst he’d ever seen. He showed me a snippet of the video and explained that not only were both my ovarian veins 3+ times the width of normal, but that the blood flow was 100% traveling down into my pelvis instead of traveling up back to my heart. My circulation in this area was almost completely not working. And it was causing my blood to pool up in my pelvis.
I explained to him that I’d been told by the other VRs that a procedure to fix this wouldn’t be covered. He confirmed that is correct, if what I’m diagnosed with is Pelvic Congestion Syndrome. But that based on the tests he had done, I also had a different diagnosis called Pelvic Venous Insufficiency, and the procedure to fix that (the same procedure) would be covered. I asked him if he thought that this could make my leg pain better, and he said it might, but he couldn’t be sure.
He explained that while they do the procedure, they’ll check for underlying causes like a kink in my veins, which are more known to cause pain down the leg or in the hip (e.g. May Thurner’s). He walked me through what they’d do to fix it: because my ovarian veins were no longer functioning, the blood had (albeit with less effectiveness) found alternate ways to return to my heart, so the procedure to fix the issue would entail sealing up the ovarian veins. Technically, it’s called an bi-lateral ovarian vein embolization. We got the paperwork done, set a date for my surgery, and I left ecstatic.
Surgery & Results
The surgery went smoothly, and the doctor confirmed there were no pinched veins—a good sign. The worst part was whatever they gave me to keep calm during (I was not fully out) made me sick on the way out. There wasn’t much pain, but my body did feel like it’d been through a lot. It took me a week or so to fully recover. At about that time, I told my husband that it felt like I had more energy. He agreed–even more so. He said it seemed like I had three times as much energy as I’d had before the procedure.
We joked that I was now the energizer bunny, but it’s hard to explain how shockingly different it was. I suddenly was able to not only get through a work day, but also handle mornings with ease, and I had enough juice left over to do something in the evenings. My weekends were no longer all recovery time. I finally had the energy to spend meaningful time with friends and family—and to begin tackling the years of neglected home projects.
We joked that I was now the energizer bunny, but it’s hard to explain how shockingly different it was.
Over the next month or so, I did a bit more research online, but couldn’t find many other accounts of people with Pelvic Venous Insufficiency having significant energy improvements. What I did find, however, were studies linking inadequate blood volume and circulation to chronic fatigue. Low blood volume is called Hypovolemia, and common symptoms include fatigue, low blood pressure, cold extremities, and rapid heart rate. These were all things I’d struggled with, but didn’t realize could be related.
Seeing the comments about rapid heart rate reminded me of when I’d gotten my first Fitbit a few years earlier. I was shocked to see the heart rate charts. They would constantly report that I’d spent 3-5 hours in fat burn mode, and sometimes even 1-2 hours in cardio when I was just working or around the house–no exercise at all. I had even brought this data to my internal medicine doctor at the time, concerned that there might an issue, but I don’t remember her giving it much thought.
I pulled out my Fitbit app to see if it had changed at all, and the results were alarming. After the surgery, I was reporting one hour of fat burn or less, and no cardio unless I was working out. See the change for yourself:
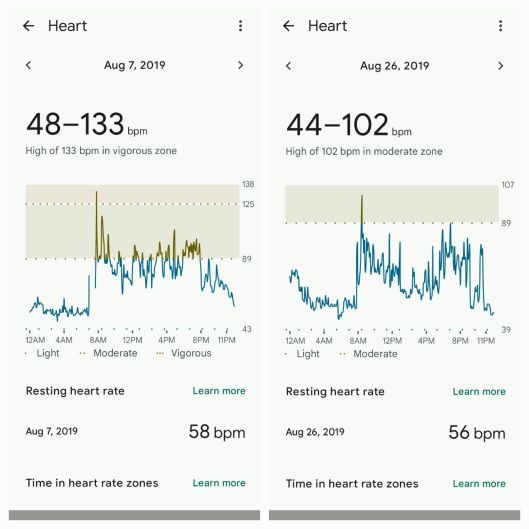
On top of the huge change in heart rate, I figured out that my blood pressure went up on average by about 10 points for both diastolic and systolic. Where as previously it was normal for me to be around 95/55, after the surgery a normal measurement would be around 105/65. I know doctors only talk about high blood pressure being an issue, but through my own research, I’d learned that low blood pressure is bad in other ways.
Unfortunately, the surgery did not eliminate my hip and leg pain. But it did reduce a significant amount of stress on my body, and made a huge improvement in my fatigue (and cold hands!). Ironically, it also drove notable improvements in my mood–I was less angry and anxious than before. Years later, after learning about the science behind stress and the adrenals, I learned this was because my body was no longer in shock all the time trying to get adequate blood and nutrients, and thus it lowered the amount of cortisone my adrenals were releasing. This is likely one key reason I flagged positive on the Adrenal Fatigue assessment. It is frustrating to say the least that it took me as long as it did to figure out and resolve this issue, but I am very lucky that I did.
I believe pelvic venous insufficiency remains under-diagnosed and poorly understood. My OBGYN who found it didn’t even mention it although I was going to them for issues in my pelvic area. And when I shared my improvements in heart rate and blood pressure with my great VR doctor, he dismissed that the surgery could drive those improvements. Being that I read it’s very common for women, especially if they have multiple child births, I’d imagine there are a lot of other women out there struggling and unaware. I hope sharing this story helps at least a few others find a path to better health.
Stay tuned for my next post, where I’ll share a few more setbacks with pain, illness, and a couple new ailments. After that, my next few posts will be sharing the remaining surprises and remarkable progress in my health journey.

fantastic! Reports Detail [Cultural Trends] in [Region] 2025 enchanting
LikeLike